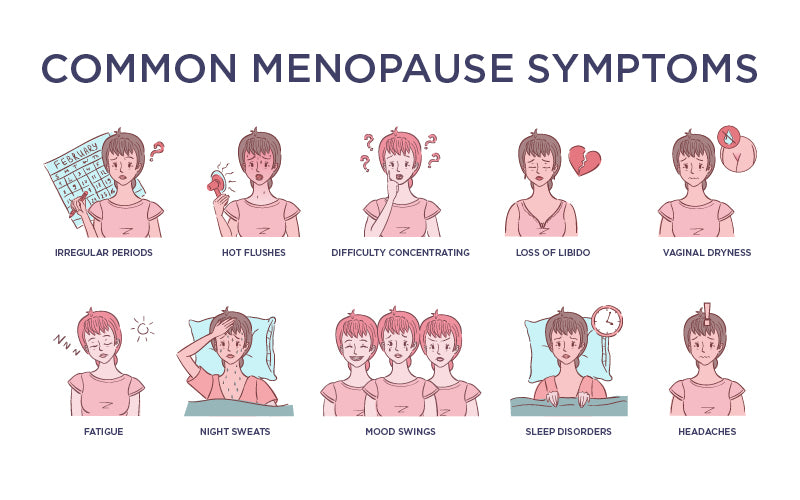
Premenstrual syndrome (PMS) affects millions of Australian women every year. Globally, this psycho-neuro-endocrine disorder affects 71-73% of Western women and 23-24% of those in non-Western cultures.
The etiology of PMS is the consequence of complex and poorly understood connections between neurotransmitters, ovarian hormones and endogenous opioid peptides, as well as prostaglandins and the autonomic, circadian, peripheral and endocrine systems. Individual biological, genetic, psychological and sociocultural factors may also play a role in the severity of symptoms. Due to these complexities, PMS has now been categorised into 5 different subtypes:
- PMS-A (Anxiety)
- PMS-C (Cravings)
- PMS-H (Hyperhydration)
- PMS-D (Depression)
- PMS-P (Pain)
PMS-A (Anxiety)
Common symptoms:
- Anxiety
- Insomnia/dyssomnia
- Irritability
- Emotional lability
- Palpitations
- Stress-induced sweating
Excess in oestrogen relative to progesterone is seen in this type of PMS. Oestrogen stimulates the brain by altering the ratio and levels of certain neurotransmitters (raises adrenalin, noradrenaline and serotonin and decreases levels of dopamine and phenylethylamine). This brain stimulation is where the symptoms of anxiety, nervous tension and mood swings are stemmed from. Excess oestrogen can block vitamin B6’s supportive actions on the body and cause blood sugar imbalances which also affect mood. Low progesterone can also leave you feeling anxious and irritated, bring about lower tolerance for stress, and cause sleep problems.
PMS-C (Cravings)
Common symptoms:
- Sugar cravings
- Increased appetite
- Headache
- Palpitations
- Increased sweating
- Moodiness
PMS-C is driven by a hormonal imbalance with its exact mechanism not clearly understood. An increase in cellular capacity to bind insulin has been postulated and a deficiency of PGE1 is known to inhibit glucose-induced insulin production. The symptoms of this type of PMS are quite similar to hypoglycemia. Low serotonin levels have also been identified in these cases which can result in a craving for sweets because carbohydrates can temporarily increase serotonin levels (pleasure pathways).
PMS-D (Depression)
Common symptoms:
- Depression
- Despair and apathy
- Crying
- Feelings of hopelessness
- Fatigue
- Insomnia
- Low libido
PMS-H (Hyperhydration)
Common symptoms:
- Oedema of hands and feet (can extend to the limbs)
- Weight gain
- Bloating
- Breast tenderness and/or swelling
- Nipple sensitivity
PMS-H is where we see the most fluid retention brought about by stress, low magnesium and high oestrogen, disrupting the normal ACTH/Aldosterone axis. A vicious cycle can occur in which the high aldosterone level increases the renal output of magnesium, further raising the aldosterone level. The balance of oestrogen and progesterone can also influence our electrolyte and fluid balance via the kidneys’ sodium regulator known as the renin-angiotensin-aldosterone system (RAAS).
Oestrogen has the ability to stimulate RAAS by inducing angiotensinogen synthesis in the liver. This process is speculated to be the underlying cause of the menstrual symptoms of bloating and weight gain. Progesterone, on the other hand, exhibits anti-mineralocorticoid activity by competing with aldosterone at the receptor level. This may favourably impact menstrual-related bloating and weight gain. These effects are mediated by endogenous progesterone.
PMS-P (Pain)
Common symptoms:
- Menstrual stomach cramping
- Aches and pains
- Lowered pain threshold
PMS-P (also known as dysmenorrhoea) is categorised as pain experienced just before and during a menstrual bleed. It typically peaks at the beginning of the period, with symptoms diminishing 48 hours after. However, it is common for symptoms to stay longer.
Symptoms of this PMS type include cramps due to distorted prostaglandin and leukotriene levels and a rise in vasopressin levels. These imbalances increase uterine resting tone, active pressure, and frequency of contractions, causing dysrhythmic uterine activity. Contractions diminish blood flow to the cells of the uterus and with a lack of oxygen, the cells increase ischemia and hypoxia of uterine tissues that trigger and heighten pain.
Getting to the bottom of things
Definitively categorising PMS can be difficult. There can be a mixture of a few types or even a possibility to present with all of the mentioned symptoms. Regardless, it is important to remember that any symptom is a little message your body is signalling to you that something isn’t quite right. PMS is common, but this doesn’t mean it has to be your ‘normal’ experience around menstruation time.
We do have several solutions for you.
- Check out our latest HAPPY HEALTHY YOU guidebook for diet and lifestyle changes that can address issues related to PMS.

- Consider taking Happy Hormones and Happy Greens as a starting point if you need additional support for PMS.
- If you feel like you need more 1.1 support then we have our online clinic with our amazing team of women's health practitioners who can guide you towards the ideal treatment plan.
REFERENCES
Vigod, S., Ross, L., & Steiner, M. (2009). Understanding and treating premenstrual dysphoric disorder: an update for the women's health practitioner. Obstetrics & Gynecology Clinics Of North America, 36(4), 907-xii.
https://pubmed.ncbi.nlm.nih.gov/19944308/
Girman, A., Lee, R., & Kligler, B. (2003). An integrative medicine approach to premenstrual syndrome. American Journal of Obstetrics and Gynecology, (5). 56.
https://pubmed.ncbi.nlm.nih.gov/12748452/
Yonkers, K. A., O'Brien, P. M., & Eriksson, E. (2008). Premenstrual syndrome. Lancet (London, England), 371(9619), 1200–1210.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3118460/
Kendler, K. S., Karkowski, L. M., Corey, L. A., & Neale, M. C. (1998). Longitudinal population-based twin study of retrospectively reported premenstrual symptoms and lifetime major depression. American Journal of Psychiatry, (9). 1234
https://pubmed.ncbi.nlm.nih.gov/9734548/
Jensen, D. V., Andersen, K. B., & Wagner, G. (1987). Prostaglandins in the menstrual cycle of women. A review. Danish medical bulletin, 34(3), 178–182.
https://pubmed.ncbi.nlm.nih.gov/3297513/








Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.