What is Polycystic Ovary Syndrome (PCOS)
By Jeff Butterworth
Polycystic Ovarian Syndrome (PCOS) is complex, involving more than just the hormones. It is common among women of reproductive age and the more you can understand what's happening within your body and why, the more power you have to improve your situation.
Don’t worry if you don’t get the whole picture. Some of the pathophysiology below is technical. But if you get the general idea that’s fine.
What is PCOS?
Polycystic Ovarian Syndrome. Yes, I realise that you've probably already done your homework; however, it's important to get a clear understanding of the full reality in a simple manner:
- PCOS affects between 10 - 20% of women and is increasing in prevalence every year.
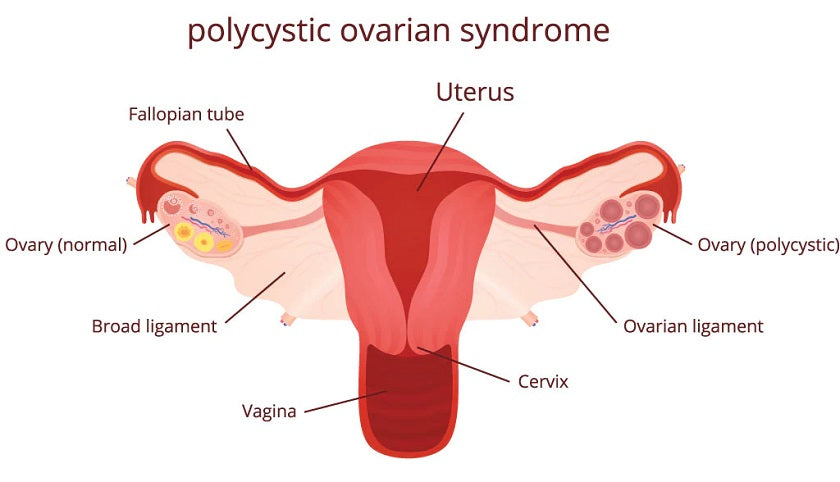
- PCOS refers to multiple cysts on the ovaries and a host of other problems that go along with them, including anovulation (lack of ovulation) and menstrual abnormalities, hirsutism (facial hair), male pattern baldness, acne, and often obesity.

- Such women may also have varying degrees of insulin resistance and an increased incidence of Type II diabetes, unfavourable lipid patterns (usually high triglycerides), and a low bone density. Laboratory tests often show higher than normal circulating androgens, especially testosterone.
- PCOS occurs when a woman doesn't ovulate, which causes a disruption in the normal, cyclical interrelationship among her hormones, brain and ovaries. Normally, the hypothalamus, a regulatory centre in the brain, monitors the hormone output of the ovaries and synchronizes the normal menstrual cycle.
- When monthly bleeding ends, the hypothalamus secretes gonadotropin-releasing hormone (GnRH), which stimulates the pituitary gland in the brain to release follicle stimulating hormone (FSH) and luteinizing hormone (LH).
These hormones direct an ovary to start making estrogen (mostly estradiol), and stimulate the maturation of eggs in about 120 follicles. The first follicle that ovulates, releasing its egg into the fallopian tube for a journey to the uterus, quickly changes into the corpus luteum, which is a factory for making progesterone, and raises progesterone's concentrations to 200 to 300 times higher than that of estradiol.
This huge surge of progesterone simultaneously puts the uterine lining in its secretory or ripening phase and turns off further ovulation by either ovary. If fertilization does not occur, the ovary stops its elevated production of both estrogen and progesterone.
The sudden fall in the concentrations of these hormones causes shedding of the blood-rich uterine lining and bleeding (menstruation). Then, in response to low hormone levels, there is a rise in GnRH and the cycle starts all over again.
But what happens to this cycle if, for some reason, ovulation is unsuccessful? For example, if the follicle migrates to the outside of the ovary, but does not "pop" the egg and release it, the follicle becomes a cyst, and the normal progesterone surge does not occur.

The lack of progesterone is detected by the hypothalamus, which continues to try to stimulate the ovary by increasing its production of GnRH, which increases the pituitary production of FSH and LH. This stimulates the ovary to make more estrogen and androgens, which stimulates more follicles toward ovulation. If these additional follicles are also unable to produce a matured ovum or make progesterone, the menstrual cycle is dominated by increased estrogen and androgen production without progesterone. This is the fundamental abnormality that creates PCOS.
Signs and Symptoms of PCOS
- Irregular menstrual cycles
- Absent period
- Anovulatory cycles
- Abnormal mid-cycle bleeding
- Excessive or heavy menstrual bleeding
- Alopecia (balding)
- Hirsutism (excessive body hair)
- Acne
- Acanthosis nigricans – a darkening of the skin in the armpits, back of the neck, or groin
- Polycystic ovaries
- History of ovarian cysts
- Mood disorders
- Obesity
- Recurrent Miscarriage
How to Diagnose PCOS
An adult woman is diagnosed with PCOS if she has at least two of the following symptoms:
- Excess androgens: Clinical or biochemical hyperandrogenism determined by the presence of total (TT) or free (FT) testosterone excess
- Ovulatory dysfunction: Characterised by oligo-amenorrhea and chronic anovulation
- Polycystic ovaries: Found on ultrasound in adult women
In addition, any diagnosis of PCOS must rule out other androgen-excess disorders.
Physicians should also screen patients for endometrial cancer, mood disorders, obstructive sleep apnoea, diabetes, and cardiovascular disease. Diagnosis of PCOS in adolescent girls should be based on clinical or biochemical signs of hyperandrogenism (after excluding other possible causes) in the presence of persistent oligomenorrhea, the task force advises.
A PCOS diagnosis during perimenopause and menopause should be based on a documented, long-term history of oligomenorrhea and hyperandrogenism in reproductive years, the report advises. A finding of PCO morphology via ultrasound would also provide supportive evidence, although the authors note this is least likely in menopausal women.
The guidelines recommend against routine ultrasound for endometrial thickness in women with PCOS. In diagnosing and treating women with PCOS, physicians should look for terminal hair growth, acne, alopecia, acanthosis nigricans, and skin tags during a physical examination, according to the new guidelines. Screening for ovulatory status using menstrual history is also recommended.
The guidelines further advise assessment of body mass index, waist circumference, blood pressure, and oral glucose tolerance. Overweight and obese patients with PCOS symptoms should be screened for obstructive sleep apnea. Both adults and adolescents should also be screened and treated for depression and anxiety.
Health and Fertility Risks Associated with PCOS
- Infertility
- Menstrual cycle irregularities
- The possible increased risk for endometrial and breast cancer due to unopposed estrogen
- Cardiovascular disease
- Diabetes
- Gestational diabetes
"It's not a pretty picture, that’s for sure, however there is a realistic and effective solution."
Can PCOS be treated?
It's not easy, but it's not that hard either. It involves a combination of diet, lifestyle, specific exercises, stress release and balancing the endocrine imbalance - which is at the core of the development of PCOS in the first place.
Health experts recommend treatment with hormonal contraceptives as the first-line therapy for menstrual abnormalities and hirsutism/acne. Exercise therapy is recommended to manage weight, alone or with a calorie-restricted diet.
The Endocrine Society task force advises against the use of metformin as a first-line PCOS treatment. However, metformin is recommended for women with PCOS and type 2 diabetes or impaired glucose tolerance, who do not succeed with weight loss and exercise. Metformin is also recommended for women who cannot take hormonal contraceptives.
For infertility, it is recommended that clomiphene citrate as a first-line treatment. For women undergoing in vitro fertilization, the guidelines provided by the Encorine Society recommend metformin as adjuvant therapy to prevent ovarian hyperstimulation.
What Now?
Women with PCOS have a hormonal imbalance, to begin with. If you'd like to try Happy Hormones, please click here.
Above all, it will reduce your PCOS symptoms at worst; and improve the condition in the best scenario. We provide the outline and the tools. You provide the willpower and motivation.
To download our free Report: "How to Manage the Symptoms of PCOS" please click the button below:

REFERENCES
Valentina Rodriguez Paris and Michael J. Bertoldo. The Mechanism of Androgen Actions in PCOS Etiology. Medical Sciences (Basel). 2019 Sep; 7(9): 89.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6780983/
Robert L. Rosenfield and David A. Ehrmann. The Pathogenesis of Polycystic Ovary Syndrome (PCOS): The Hypothesis of PCOS as Functional Ovarian Hyperandrogenism Revisited. Endocrine Reviews. 2016 Oct; 37(5): 467–520.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5045492/






Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.