Each and every one of us knows from personal experience that anxiety, nervousness, and even heartache can manifest as physical pain or discomfort in the gut. Getting ‘butterflies in your stomach’ is the best way to describe this and the fact that these sensations frequently occur together is no coincidence.
Did you know that our digestive tract harbours ten times more microorganisms than the number of cells that make up the human body?
These microorganisms or bacteria are collectively known as the microbiome. It develops soon after birth and is integral to immune function, digestion and, of course, brain health. Likewise, we now know that there are more happy hormone receptors in our gut than we have in our brain (serotonin particularly). This simply provides further insight as to why so many people feel stress in their tummies first before anywhere else.
Is Your Low Mood Caused by Poor Digestion?
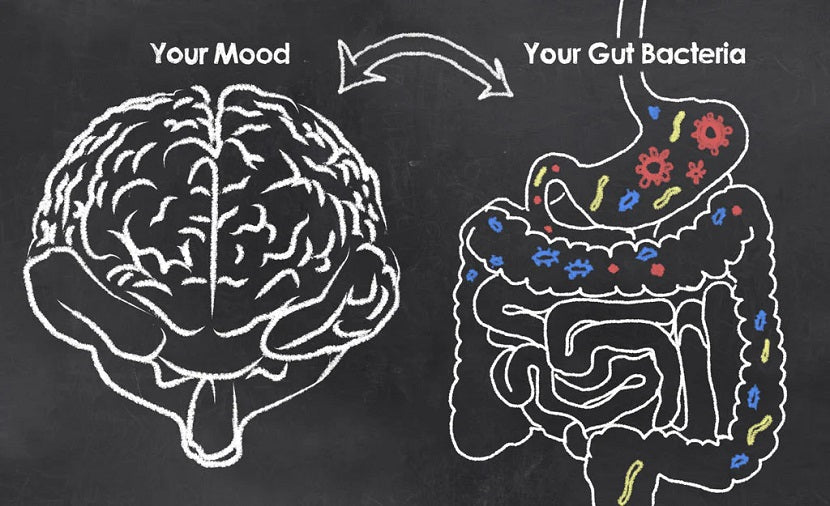
In Neuroscience, there is something called the ‘gut-brain axis’. Essentially it’s the invisible connection between our brain and all the bacteria in our digestive tract. So why is this axis quite vital to mental and emotional wellbeing? Well in some way, this microbiome actually communicates with our nervous system, affecting how we behave and respond to stress. It even influences how we react to therapy and anti-anxiety medications or antidepressants.
A 2012 study conducted in Ireland revealed that serotonin levels in the brain are regulated by the number of healthy gut bacteria early in life. Furthermore, a study from the Journal of Molecular Psychiatry found that normal adult brain function depends on the presence of healthy gut microbes during childhood development.
If better bacteria in our gut can improve mood, how can we achieve this in our everyday lives?
How to elevate your mood naturally
To start off, let’s address any setbacks originating from birth. For instance, were you or your child born via caesarean delivery? If so, it’s likely you missed out on the big mouthful of bacteria we acquire when emerging through the vaginal canal. Infants delivered through a C-section are more likely to develop food intolerances, allergies and skin conditions like eczema, as well as potential behavioural issues.
So how do you fix this? It’s as easy as putting powdered probiotics on the mother’s nipple when nursing infants or giving this directly as a supplement in water or milk. For adults, on the other hand, the gut-brain relationship and how a healthier digestive tract may improve stress levels are clear. Let this knowledge propel you toward making changes in your everyday life by being proactive about the following healthy practices.
1: Follow a probiotic-rich diet
Even if you weren’t born via caesarean section, don’t forget that stress alone can cause bad bacteria to develop in your digestive tract. Combating this with a good dose of friendly bacteria from fermented foods is key.
Aim for a few times per week and go for options like miso, kombucha, kimchi, sauerkraut, tempeh or natto. Making your own coconut water kefir is also simple and effective to reestablish healthy live probiotics. A simple way to build healthy probiotics is by taking fermented products and foods which contain LIVE probiotics that are active and ready to work the minute they hit your system.
Our newest Happy Digestion formula can also help. It's packed with prebiotics, probiotics, and postbiotics to optimize gut health.

2: Consume more anti-inflammatory foods
What exactly are anti-inflammatory foods? Well, you can actually find lots of them in your pantry or fridge! Omega 3 fatty acids like those found in oily fish, nuts, flaxseed, hemp, chia seeds, and avocado are just a few great examples.
A diet designed specifically to reduce inflammation also suggests avoiding foods that trigger an inflammatory response. This means cutting down on processed foods, excess sugar, alcohol or anything else you know you might react to. On the other hand, moderate portions of simple, easily digested foods like cooked veggies, grains and protein can be beneficial for your gut.
Bloating, gas, reflux, diarrhoea and nausea are clear indications of inflammation or fermentation in the gut. All these symptoms will affect your microbiome and eventually your mood and happiness!
Our latest HAPPY HEALTHY YOU book is a valuable resource to firstly understand how your body works, and then take proactive steps to improve your health. It also includes over a hundred of our curated recipes that can help you in your journey to optimum health and wellness!
3: Exercise daily
We know that exercise releases the chemical endorphin, one of the so-called ‘happiness hormones’. Additional research now also tells us that exercise early in life actually alters our microbiome, which in turn optimizes brain health and even our metabolism. Regular exercise has also been studied to improve and enrich the diversity of the microbiome.
Do you feel as though exercise is a type of meditation? I do, and it makes sense that research is also telling us that mindfulness meditation has the same effect. So don’t waste time and get started!
4: Speak up and get help
Lastly, don’t forget to speak up if you’re struggling. A recent meta-analysis of 41 studies found that entering the ‘gut-brain axis’ via psychotherapy effectively reduced the symptoms of Irritable Bowel Syndrome (IBS) in both the short and long term by 75 percent.
Key Takeaway
If we hypothesize that IBS is the result of an altered ‘gut-brain axis’, then I think it’s safe to say that more focus on mindfulness and creating a healthier and balanced mind will absolutely improve the state of your digestive health.
If you want to learn more about how to improve your gut health and microbiome, see this article on probiotics and prebiotics. You can also join any of our private HHY Facebook groups where we share vital information on this topic every week.

REFERENCES
Appleton J. (2018). The Gut-Brain Axis: Influence of Microbiota on Mood and Mental Health. Integrative medicine (Encinitas, Calif.), 17(4), 28–32.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6469458/
Bell, V., Ferrão, J., Pimentel, L., Pintado, M., & Fernandes, T. (2018). One Health, Fermented Foods, and Gut Microbiota. Foods (Basel, Switzerland), 7(12), 195.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6306734/
Carabotti, M., Scirocco, A., Maselli, M. A., & Severi, C. (2015). The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Annals of gastroenterology, 28(2), 203–209.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367209/
Monda, V., Villano, I., Messina, A., Valenzano, A., Esposito, T., Moscatelli, F., Viggiano, A., Cibelli, G., Chieffi, S., Monda, M., & Messina, G. (2017). Exercise Modifies the Gut Microbiota with Positive Health Effects. Oxidative medicine and cellular longevity, 2017, 3831972.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5357536/
Neu, J., & Rushing, J. (2011). Cesarean versus vaginal delivery: long-term infant outcomes and the hygiene hypothesis. Clinics in perinatology, 38(2), 321–331.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3110651/








Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.